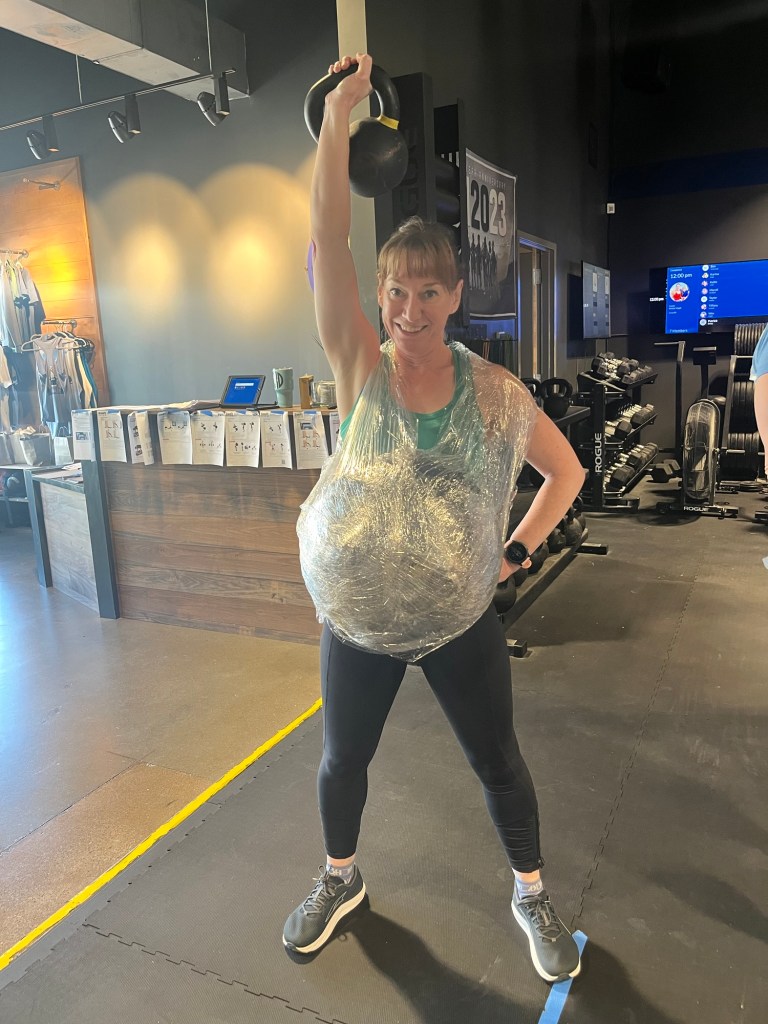
I recently showed up to my gym for what I thought was a regular class, only to find out it was a pregancy inspired workout in honor of one of our pregnant classmates. So we all strapped on wallballs (mine weighed 14 pounds) and proceeded to do a variety of sprints, pullups and kettlebell swings.
It remided me how challenging it can be to exercise with a bump, but also how important it is to stay as active as you can through the process.
Exercise during pregnancy has shown to help reduce excess weight gain, preeclampsia, c-section and the risk for gestational diabetes. Additionally, exercise in pregnancy and phyical activity postpartum can reduce your risk of postpartum depression.
Current recommendations for healthy women by the US Department of Health and Human Services:
- Healthy women who are not already highly active or doing vigorous-intensity activity should get at least 150 minutes of moderate-intensity aerobic activity a week during pregnancy and the postpartum period. Preferably, this activity should be spread throughout the week {i.e. 30 minutes, 5 days a week as a goal}.
- Pregnant women who are highly active can continue physical activity during pregnancy and the postpartum period assuming that they remain healthy and discuss with their healthcare provider how and when activity should be adjusted over time.
So how does this translate into real life?
6 Tips for Safe Exercise During Pregnancy
1. Start slow. Even if you haven’t been previously active; walking, pilates and swimming are great activities that you can safely start during pregnancy. Begin with 10-15 minutes a day and add 5 minutes a week until you reach 30 minutes a day.
2. Don’t fall down. Activities such as horseback riding, skiing, box jumps and hockey which have a high risk of falling or trauma should be avoided after the first trimester.
3. Don’t push it. If during exercise you begin experiencing chest pain, contractions or vaginal bleeding, then stop and consult your doctor. Generally, 25 pounds should be your lifting limit, however, take your pre-pregnancy conditioning regimine into account. An example being a crossfitter who can normally squat 250 lbs could probably lift 150 lbs without straining, whereas a non-athlete may feel strained when lifting 20 lbs.
4. On a scale of 1 to 10, you want to workout with an exertion level of 6 to 7. You want to have your heart rate up, but still be able to talk during the activity. Ideally exercise 30-60 minutes a day.
5. Check with your doctor if you are a professional/competitive athlete {if you work out more than an hour a day} so she can help to determine the safety of your specific situation.
6. Don’t lay flat after 20 weeks. Cardiovascular changes in the body and the position of the uterus reduce the blood flow to the uterus if you lay flat after 20 weeks.
Pregnancy complications that make exercise contraindicated:
- Heart disease
- Severe lung disease
- Cerclage
- Preterm labor {in current pregnancy}
- Placenta previa {> 26 weeks}
- Unexplained vaginal bleeding
- Preeclampsia
If you are active when you start pregnancy, that is great. Continue your routine throughout pregnancy, if you have no contraindications. If you are not active, look for ways to get moving and incorporate exercise into your daily activities.

